Background: The challenge of non-communicable diseases
Non-communicable diseases (NCDs), principally cardiovascular diseases, diabetes, cancers, and chronic respiratory diseases, are the leading causes of death globally, killing more people each year than all other causes combined. NCDs caused an estimated 35 million deaths in 2005. This figure represents 60% of all deaths globally, with 80% of deaths due to non-communicable diseases occurring in low- and middle-income countries. About one fourth of global NCD-related deaths take place before the age of 60.
The combined burden of these diseases is rising fastest among lower-income countries, populations and communities, where they impose large, avoidable costs in human, social and economic terms. Patients and their families are pushed into poverty because of catastrophic health expenditures and countries are spending a large part of their health budget on chronic conditions. A recent Harvard University study estimates that over the next 20 years, non-communicable diseases will cost the global economy more than $30 trillion, representing 48 per cent of the global GDP in 2010.
Total deaths from non-communicable diseases are projected to increase by a further 17% over the next 10 years. The rapidly increasing burden of these diseases is affecting poor and disadvantaged populations disproportionately, contributing to widening health gaps between and within countries. Despite their rapid growth and inequitable distribution, much of the human and social impact caused each year by NCD-related deaths could be averted through well-understood, cost-effective and feasible interventions.
The four ‘major’ NCDs – cardiovascular diseases, chronic respiratory diseases, diabetes and cancer – are caused to a large extent, by four behavioural risk factors that are pervasive aspects of economic transition, rapid urbanization and 21st-century lifestyles: tobacco use, unhealthy diet, insufficient physical activity and the harmful use of alcohol. The greatest effects of these risk factors fall increasingly on low- and middle-income countries, and on poorer people within all countries, mirroring the underlying socioeconomic determinants. Among these populations, a vicious cycle may ensue: poverty exposes people to behavioural risk factors for NCDs and, in turn, the resulting NCDs may become an important driver to the downward spiral that leads families towards poverty. As a result, unless the NCD epidemic is aggressively confronted in the most heavily affected countries and communities, the mounting impact of NCDs will continue and the global goal of reducing poverty will be undermined.
As the magnitude of the NCD epidemic continues to accelerate, the pressing need for stronger and more focused international and country responses is increasingly recognized by Member States. Since the WHO Secretariat presented its Global Strategy for the Prevention and Control of Non-communicable Diseases to the World Health Assembly in 2000, many resolutions on the topic were adopted and many meetings held, most recently the High-level Meeting of the United Nations General Assembly on the Prevention and Control of Non-communicable Diseases. We have prepared a presentation which provides an overview of all the relevant resolutions, documents and political declarations. It also summarizes the aspects of relevance for members of the PHM, focusing on what has been said on the social determinants of health, access to medicines, integration, sustainable financing and accountability.
However, despite abundant evidence of their negative impact, policy-makers still fail to regard NCDs as a global or national health priority. Incomplete understanding and persistent misconceptions continue to impede action. Although the majority of NCD-related deaths, particularly premature deaths, occur in lowand middle-income countries, a perception persists that NCDs afflict mainly the wealthy. Other barriers include the point of view of NCDs as problems solely resulting from harmful individual behaviours and lifestyle choices, often linked to victim ‘blaming’. The influence of socioeconomic circumstances on risk and vulnerability to NCDs and the impact of health-damaging policies are not always fully understood; they are often underestimated by some policy-makers, especially in non-health sectors, who may not fully appreciate the essential influence of public policies related to tobacco, nutrition, physical inactivity and the harmful use of alcohol on reducing behaviours and risk factors that lead to NCDs. Effective interventions, such as tobacco control measures and salt reduction, are not implemented on a wide scale because of inadequate political commitment, insufficient engagement of non-health sectors, lack of resources, vested interests of critical constituencies, and limited engagement of key stakeholders.
Reducing exposure to the risk factors for NCDs and their determinants is also not enough. Improved health care, early detection and timely treatment is another necessary aspect of reducing the impact of NCDs. However, appropriate care for people with NCDs is lacking in many settings, and access to essential technologies and medicines is limited, particularly in low- and middle-income countries and populations. Health systems need to be further strengthened to deliver an effective, realistic and affordable package of interventions and services for people with NCDs.
We need to change the way policy-makers perceive NCDs and their risk factors, and how they then act. Concrete and sustained action is essential to prevent exposure to NCD risk factors, address social determinants of disease and strengthen health systems so that they provide appropriate and timely treatment and care for those with established disease.
Sources:
WHO Global Status Report on Non-communicable Diseases
WHO 2008-2013 Action Plan on the Global Strategy for the Prevention and Control of Non-communicable Diseases
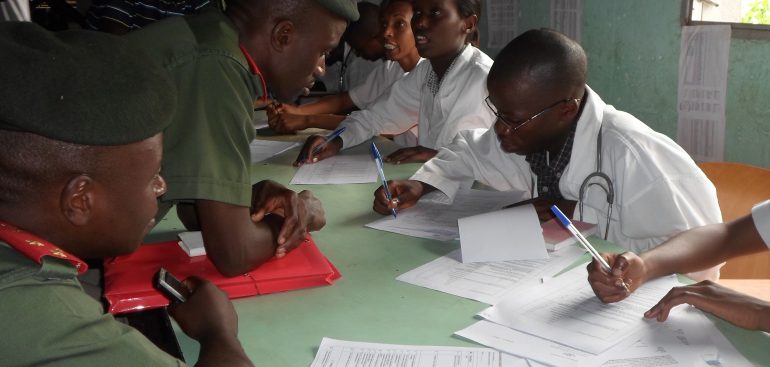
In the country, even few researchers have been done in this domain. In our observation, NCDs remain a burden. We are active in the ground through advocacy and health education. Village health action team has organized twelve campaigns in rural, semi-urban and urban areas to raise awareness on the growing of NCDs.
We have been working with ministry of health and other civil society organizations to raise the voices of people living with NCDs and have reached more than 120, 000 people. In the near future, our platform will work on different sides such as:
- reduce tobacco use by implementing effective mass-media campaigns that educate the public about the harms of smoking/tobacco use and second-hand smoke.
- reduce harmful use of alcohol: our plan is to do an advocacy so that government enforce restrictions on the physical availability of alcohol in sales outlets.
- reduce physical inactivity: our approach is to implement a community-wide public education and awareness campaigns for physical activity, including mass-media campaigns combined with other community-based education, motivational and environmental programmes aimed at supporting behavioural change around physical activity levels.
- Reduce unhealthy diet: we will focus on education by reducing salt intake through behavior change communication and mass media campaigns
- Reduce by education risk factors of cardiovascular diseases and diabetes
- Prevent cancer: village health action will mainly focus on breast and cervical cancer by doing mass media campaigns raise awareness on risk factors and the importance of early detection.
The best way to tackle NCDs in low income countries is to conduct early prevention at the grassroots level.